Like many of those who suffer from opioid dependency, Talia Eisenberg's story of healing began with, well, a need to heal—from a dental procedure, that is. She'd been prescribed opiates to treat the pain of her recovery and soon she learned they soothed not only her toothache but also the lifelong anxiety she'd dealt with since childhood.
"It went from that to heroin," she says, and by her early 20s, she'd cycled through four or five traditional rehabs. "Part of me wanted to stop, and another part of me didn't. I would need to have an opiate even after being sober for 30 days during one of these programs." As Eisenberg explains from her own experience, addiction is a complex creature: "There's both a physical dependency when it comes to opiates—you'll be very sick if you don't take an opiate within a certain amount of time—and it's also psychological—it's an obsession, you can't stop thinking about it, you need it to function and feel normal."
The only thing that would catalyze her recovery from opioid dependency was psychedelics. "It was nothing short of a miracle to find ibogaine," says Eisenberg, who was able to turn her life around following treatment with what's known to be among the world's most intense entheogens. "That obsession [with opioids] plus the physical cravings and withdrawal was 90 percent ameliorated," she recalls of the period following a 30-hour session with the alkaloid derived from the West African iboga plant. "You get a level of clarity around your life and the underlying reasons why you use drugs in the first place, which is something you can't get from most rehab programs."
Psychedelics May Help Uncover Key Insights Needed to Heal
Self-work and investigation that might otherwise take years to uncover all come to the surface in a 30-hour ibogaine session, shedding light on your points of both trauma and healing, Eisenberg explains. "I saw how my grandparents and what they went through in the Holocaust is in me, that pain and the suffering of humanity and my family. It made me want to live life fully and not poison myself but to give back and make a difference. That's a powerful component in the healing, as well."
Following her ibogaine treatment, Eisenberg left her home in New York City and moved to Boulder, where she began spending more time in nature, practicing yoga, doing therapy, and ultimately enrolling in school—all part of the ibogaine integration process. In the early days of her recovery, she also did periodic ayahuasca dietas with the Shipibo tribe in Peru about once a year. "It helped me do a lot of clearing," she says. "As a former drug addict, we need positive rituals. For me, the old ritual was the very ritualistic use of drugs, whether it was cocaine or opiates. Ayahuasca provided me the opportunity to switch that for a positive ritual—not in a way that was every weekend, but [sporadically] with reverence and integration in between."
The genesis of Talia's problematic relationship to opioids is at this point a classic American tale. Those who have been "unsuccessful in being medically detoxed or transitioned in their medications may have a sticky attachment to their pain meds and are at high risk of developing a more entrenched opioid addiction or transitioning to street opioids," notes addictions researcher Tashia Petker, a Ph.D. student in clinical psychology at the University of British Columbia.
This is the population to which Petker and her research team are hoping to apply psilocybin therapy. There's a misconception that most people who struggle with opioids are street or recreational users, but "a lot of them started off with prescriptions for pain medications and there are certain susceptibilities that people have psychologically for addiction risk," she explains.
What Psychedelics Are Used to Treat Opioid Addiction?
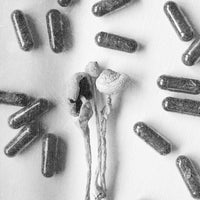
Indeed, there's a gamut of psychedelic substances that can be used to treat those who struggle with opioids—despite that, from outside the alternative therapy space, Eisenberg notes, it might seem counterintuitive to treat a drug problem with another "drug."
But this is exactly the promise of psychedelic-assisted therapy, using psilocybin (the active compound in magic mushrooms), ayahuasca (a brew of two plants, which contains DMT), ibogaine, and other compounds that "agonize" the brain's 5H2A receptors. That's all to say, psychedelic therapy to treat addiction isn't about replacing one substance with another, but using the latter just one or a few times—in conjunction with substantial lifestyle changes—to catalyze the recovery process. And therein lies the potential of psychedelics in treating individual addiction, and perhaps even combating America's opioid crisis at large.
Can Psychedelics Help in the Fight Against the Opioid Epidemic?
Because addiction is so complex it calls for a complex treatment option—one that touches upon the biochemical, physiological, psychological, and spiritual factors that lend themselves to opioid dependence. As psychiatrist, Dr. Simon Ruffell MD, Ph.D., explains, addiction is the result of dopamine release in the mesolimbic system, whereby drugs of abuse (or other addictive things, from cigarettes to social media) signal the release of dopamine in the brain's dopamine, or reward pathway (also known as the pleasure sensor).
A senior research fellow at the University of Melbourne, co-founder of Onaya Health, and CMO of Psychae Institute and Heroic Hearts UK, Ruffell—who primarily studies ayahuasca—explains the hypothesis that psychedelics might exert anti-addictive properties by reducing the levels of dopamine in the brain via the mesolimbic pathway and taking effect on the serotonin receptors (known as the 5HT2A receptors). By acting upon, and more specifically agonizing these serotonin receptors—that is, binding to and acting like the receptors do themselves—psychedelics may halt the natural process of addiction.
"In particular, working with ayahuasca emphasizes the psychological processes that are at play as well as the biochemical processes with addiction," says Ruffell. "From research, we see that ayahuasca seems to force people to confront or face themselves and it forces them to have a greater personal awareness and that can even work to achieve reconstruction of awareness and nature of oneself through the participants returning to their past, reassessing their experiences, and get to new perspectives or insights that might reveal particular patterns of behavior." In this way, they may question why they feel the need to take opiates.
This doesn't just happen with ayahuasca though. "One thing that seems to be common among all psychedelics—from ayahuasca to psilocybin to LSD—is that when you take them, people can have transcendental, mystical experiences," he adds. "These spiritual experiences seem to evoke change by allowing individuals to change their personal awareness and self-perception and even their worldviews. It may well be as a result of these spiritual experiences that a personal transformation occurs and craving for drugs is eliminated."
Moreover, with a psychedelic, an individual might become more conscious of repressed memories, re-experience the emotions associated with them, and reprocess these memories in a more constructive way—rather than escaping the constant plague of trauma with the numbness of an opioid high.
Psychedelics Can Only Do so Much—Integration and Accountability Are Essential
But psychedelics are not a magic bullet, and aside from the psychological, spiritual, and pharmacological mechanisms of action, a patient must be motivated to make the changes that the medicine might show them are necessary; but the psychedelic itself does not make those changes. That's why it's important to have a psychedelic integration strategy, along with a support network, that keeps a person from falling back into old habits (for example, why Talia moved from NYC to Boulder). In the Western paradigm of health, Ruffell explains, the doctor gives the patient a pill and they have little responsibility themselves to do much else to mitigate their symptoms aside from taking the medicine; however, with psychedelics, it's the opposite: "The participant gets insights from the psychedelic session and they have to go make that change. There has to be that motivation, that willingness to change."
As Petker explains, especially for opioid-dependent chronic pain patients, the spiritual aspects of a psychedelic experience foster a deeply meaningful experience and may enable patients to be comfortable in their bodies for the first time in years—and that alone could help motivate them to make consistent changes. Psychedelics may show a person the greater meaning in life, which in turn provides a sense of energy and enthusiasm that helps mitigate their pain from a more spiritual level. "It helps them live their life more fully," says Petker.
For Eisenberg, it was both the insights and chemical shift that ibogaine gave her which put her on the path to recovery. Ibogaine in particular is able to reset the body's opioid receptors, putting a dent in cravings and acute withdrawals. At the same time, it offered a sense of mystical rejuvenation. "In a 12-Step program, you get that spiritual awakening when you get to Step 12," says Eisenberg, "but here you have the awakening first, and you can use that to change your life while you don't have cravings or acute relapse and do have a window of rapid detox."
Eisenberg goes on to explain the potential for ibogaine (and other psychedelics) to put a person in connection with their "highest, best self," while also activating the brain's GDNF pathway—essentially, signaling the release of neurochemicals responsible for a childlike "feeling of joy and curiosity." While other psychedelics exit the body quickly, ibogaine activates this GDNF (which is otherwise released up till the age of 7) for many months to come, offering a neurological cushion during the habit-interrupting integration period.
For Eisenberg, the integration of her ibogaine experience and recovery has been the motivation to give back to others. She's since co-founded her own ibogaine clinic in Mexico called Beond, and advocates on the topic. Drugs and medicines, from downers to uppers to psychedelics can all be used to mitigate pain and offer a shift in awareness, but the question, as Eisenberg says, is one of if it's "a tool to go within or are you running? Then it becomes a drug that's harmful because you're using it to escape. If you're using it to intentionally sit with yourself and go inward to heal your wounds, then it's much different."
Madison Margolin is an author and journalist covering psychedelics and spirituality. Co-founder of the Jewish Psychedelic Summit and DoubleBlind Magazine, she is currently a contributing editor to Ayin Press and Lucid News, and hosts a podcast called Set & Setting on the Be Here Now Network. Her writing has also been featured in Rolling Stone, Playboy, Vice, and other publications.
Photo by Christopher Ott on Unsplash
Read More: What Psychedelic Researchers Are Learning About Mental Health
Read More: How to (Easily) Support Sacred Plant Medicine
Listen: The Power of Psychedelic Retreats with Neil Markey